The prevalence of HO in patients with traumatic brain injury (TBI) has been reported to range from 11% to 77% but is clinically relevant in 10-20% 2-8
Heterotopic Ossification
Date Published: July 10, 2020
Overview
Definition
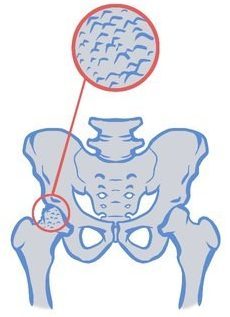
Heterotopic Ossification (HO) is a process whereby true mature lamellar bone forms ectopically within tissues where bone formation does not usually occur.1
Prevalence
Etiology
- Osteoblastic cells, in response to some osteogenic factor released by the brain trauma, undergo differentiation into highly metabolically active ectopic bone within soft tissues around hips, shoulders and elbows 9
- Ectopic osteoid matrix reaches full calcification within weeks while osseous reorganization to mature trabecular bone occurs over months 9
Risk Factors
- Skeletal trauma
- Diffuse axonal injury
- Spasticity
- Mechanical ventilation
- Duration of coma
- Spasticity
- Prolonged immobilization
- Injury severity
10,11
Clinical Features

HO formation can begin early (2-3 weeks post-injury), however, symptoms may not present until later (3-12 weeks post-injury). The joints most commonly affected are the hips, shoulders and elbows. Rarely are the knees affected. 3,12-14 Trauma to the area increases the likelihood of developing HO.
Presenting symptoms may include:
- Warm, swollen, and painful joint
- Decreased range of motion in the joint 15
- Palpable mass
- Pain at area of inflammation
Assessment
Individuals with traumatic brain injury (TBI), especially those with severe injury, should be regularly assessed for the possible presence of heterotopic ossification, The sites most frequently affected following TBI are the hips, elbows, shoulders and knees.7
History
- Prior history of HO
- Recent development of joint swelling or pain
- Later development of joint restriction
- History of fractures or musculoskeletal trauma
- Severity of the brain trauma
- Time of pain and swelling post injury
Physical Exam
- Full joint exam, including range of motion looking for swelling, warmth, pain and restricted range of motion
OSCE Examination Guides
Hip Joint
Elbow Joint
Shoulder Joint
Knee Joint
Screening
There are no specific screening tests for heterotopic ossification.
Diagnostic Testing
Early diagnosis of heterotopic ossification following traumatic brain injury should involve a three-phase bone scan. 7
During the initial presentation, plain radiographs may be negative and will usually remain normal for 2-6 weeks after the start of clinical symptoms. The triple phase technicium-99 bone scan remains the diagnostic gold standard. The test is positive if there is increased uptake during the first and second phases of the study. It typically becomes positive when clinical features appear (i.e., before findings show up on radiographs.
Bone scintigraphy/bone scans
- Triple phase bone scan using technetium-99 diphosphonate (TC-99) is the gold standard
- Increased uptake is seen in areas of active bone growth during first and second phases of the bone scan
Computed Tomography
- Able to confirm diagnosis, determine localization and extent of HO formation, important to guide surgical excision
Ultrasound
- Portable and capable of bedside detection, non-invasive, low-risk and cost-effective – ideal for early detection
X-ray
- Lacks specificity in early phases when soft tissue calcification has not yet occurred
- 7-10 days after initial symptoms, signs of HO may appear on radiographs, although it may take longer
Laboratory Investigations
- Serum alkaline phosphatase – levels may be elevated prior to symptoms
- Creatine kinase – elevated in HO but non-specific
- Erythrocyte sedimentation rate
- C-reactive protein elevated early on
Diagnosis
A diagnosis of HO can be made by a positive CT scan, bone scan, or ultrasound. The diagnostic process typically starts with a clinical examination when HO is suspected; signs and symptoms indicating possible HO are restricted range of motion, swelling, warm, or painful joints. At this stage the presence of HO should be confirmed through a secondary assessment (positive scan result), with the assessment interpreted by an appropriately trained individual, such as a radiologist.
Diagnostic Criteria
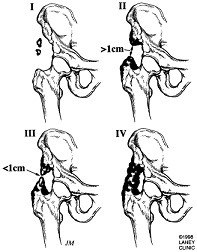
The Brooker classification 16 system is the most widely used.
Class I
- Islands of bone within soft tissues about the hip
Class II
- Bone spurs from the pelvis or proximal end of the femur with at least 1cm between opposing bone surfaces
Class III
- Bone spurs from the pelvis or proximal end of the femur with less than 1cm between opposing bone surfaces
Class IV
- Bony ankylosis of the hip
Differential Diagnosis
- Dependent edema
- DVT
- Local trauma
- Fracture
- Varicose veins
- Superficial thrombophlebitis
- Achilles tendonitis
- Ruptured Baker cyst
- Cellulitis
- Lymphedema
- Arterial insufficiency
- Hematoma
Complications
- Compression of blood vessels and nerves
- Breakdown of associated tissue
- Restricted motion
- Loss of function
- Joint ankylosis
8
Management
Non-pharmacological Interventions
Physiotherapy and Range of Motion Exercises
- Passive range-of-motion exercises are maintain joint range of motion and do not exacerbate HO.
- ROM must be gentle and within available range, aggressive ROM can worsen HO. 17
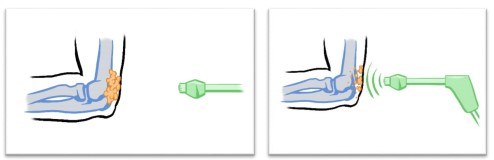
Shockwave Therapy
- Shock wave/vibration therapy seeks to erode unwanted formations of bone. 18
Radiation Therapy
- Radiation therapy is designed to disrupt mesenchymal stem cell differentiation into osteoblasts during the early phases of HO. 19
| Intervention | Effect | Level of Evidence |
|---|---|---|
| Physiotherapy/range of motion exercises* | + | 4 May improve range of motion and prevent bony ankyloses. |
| Shockwave Therapy | + | 4 May reduce pain associated with HO. |
| Radiation Therapy | + | 4 May improve range of motion and prevent further formation of HO. |
*Recommended by the INESSS-ONF Clinical Practice Guidelines
Pharmacological Interventions
Etidronate
- Works by preventing the aggregation, growth, and mineralization of calcium hydroxyapatite crystals, which are essential for bone formation.
- Considered controversial and has been associated with osteomalacia.
- A single prospective study found reduced rates of HO formation in those with an ABI compared to controls.23
Non-Steroidal Anti-Inflammatory Drugs
- There is no evidence for NSAIDs in a population with ABI
| Intervention | Effect | Level of Evidence |
|---|---|---|
| Nonsteroidal anti-inflammatory drugs* | UC | N/A Although used clinically, NSAIDs have not been studied in a population with ABI. |
| Etidronate Disodium* | + | 2 May reduce the incidence of HO when compared to placebo in patients with severe head injury. |
*Recommended by the INESSS-ONF Clinical Practice Guidelines
Surgical Interventions
Surgical excision of heterotopic ossification should be considered at a later stage in individuals with traumatic brain injury. 7
Multiple studies have found positive results on range of motion, functioning, and decrease in recurrence after the surgical excision of HO. 20-22
| Intervention | Effect | Level of Evidence |
|---|---|---|
| Surgical excision | + | C May improve range of motion. Early surgical excision does not increase recurrence risk. |
Resources
INESS-ONF Clinical Practice Guidelines for the Rehabilitation of Adults with Moderate to Severe TBI
ERABI Module
ERABI Guidebook
OSCE Examination Guides
References
1. Watanabe, Sant. Common medical complications of traumatic brain injury. Physical Medicine and Rehabilitation: state of the art reviews. 2001;15:283-299.
2. Dizdar D, Tiftik T, Kara M, Tunc H, Ersoz M, Akkus S. Risk factors for developing heterotopic ossification in patients with traumatic brain injury. Brain injury. 2013;27(7-8):807-811.
3. Garland D, Blum C, Waters R. Periarticular heterotopic ossification in head-injured adults. Incidence and location. Journal of Bone and Joint Surgery - Series A. 1980;62(7):1143-1146.
4. Rogers RC. Heterotopic calcification in severe head injury: a preventive programme. Brain injury : [BI]. 1988;2(2):169-173.
5. Sarafis KA, Karatzas GD, Yotis CL. Ankylosed hips caused by heterotopic ossification after traumatic brain injury: a difficult problem. The Journal of trauma. 1999;46(1):104-109.
6. Sazbon L, Najenson T, Tartakovsky M, Becker E, Grosswasser Z. Widespread periarticular new-bone formation in long-term comatose patients. The Journal of bone and joint surgery British volume. 1981;63-b(1):120-125.
7. Simonsen LL, Sonne-Holm S, Krasheninnikoff M, Engberg AW. Symptomatic heterotopic ossification after very severe traumatic brain injury in 114 patients: incidence and risk factors. Injury. 2007;38(10):1146-1150.
8. Zychowicz ME. Pathophysiology of heterotopic ossification. Orthop Nurs. 2013;32(3):173-177.
9. Cullen N, Taggart C. Heterotopic Ossification. Manual of Traumatic Brain Injury Management. 2011:316.
10. Bargellesi S, Cavasin L, Scarponi F, et al. Occurrence and predictive factors of heterotopic ossification in severe acquired brain injured patients during rehabilitation stay: cross-sectional survey. Clinical Rehabilitation. 2018;32(2):255-262.
11. Huang H, Cheng WX, Hu YP, Chen JH, Zheng ZT, Zhang P. Relationship between heterotopic ossification and traumatic brain injury: Why severe traumatic brain injury increases the risk of heterotopic ossification. Journal of Orthopaedic Translation. 2018;12:16-25.
12. Garland DE. A clinical perspective on common forms of acquired heterotopic ossification. Clinical orthopaedics and related research. 1991(263):13-29.
13. van Kampen PJ, Martina JD, Vos PE, Hoedemaekers CW, Hendricks HT. Potential risk factors for developing heterotopic ossification in patients with severe traumatic brain injury. The Journal of head trauma rehabilitation. 2011;26(5):384-391.
14. Vanden Bossche L, Vanderstraeten G. Heterotopic ossification: a review. Journal of rehabilitation medicine. 2005;37(3):129-136.
15. Pape HC, Marsh S, Morley JR, Krettek C, Giannoudis PV. Current concepts in the development of heterotopic ossification. The Journal of bone and joint surgery British volume. 2004;86(6):783-787.
16. Brooker AF, Bowerman JW, Robinson RA, Riley LH, Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. The Journal of bone and joint surgery American volume. 1973;55(8):1629-1632.
17. INESSS-ONF. Clinical Practice Guideline for the Rehabilitation of Adults with Moderate to Severe TBI. Ontario Neurotrauma Foundation. https://braininjuryguidelines.org/modtosevere/. Published 2015. Accessed 2019.
18. Reznik JE, Biros E, Lamont AC, et al. A preliminary investigation on the effect of extracorporeal shock wave therapy as a treatment for neurogenic heterotopic ossification following traumatic brain injury. Part I: Effects on pain. Brain Injury. 2017;31(4):526-532.
19. Balboni TA, Gobezie R, Mamon HJ. Heterotopic ossification: Pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. International journal of radiation oncology, biology, physics. 2006;65(5):1289-1299.
20. Pansard E, Schnitzler A, Lautridou C, Judet T, Denormandie P, Genet F. Heterotopic ossification of the shoulder after central nervous system lesion: indications for surgery and results. Journal of shoulder and elbow surgery. 2013;22(6):767-774.
21. Fuller DA, Mani US, Keenan MA. Heterotopic ossification of the shoulder in patients with traumatic brain injury. Journal of shoulder and elbow surgery. 2013;22(1):52-56.
22. Genet F, Chehensse C, Jourdan C, Lautridou C, Denormandie P, Schnitzler A. Impact of the operative delay and the degree of neurologic sequelae on recurrence of excised heterotopic ossification in patients with traumatic brain injury. The Journal of head trauma rehabilitation. 2012;27(6):443-448.
23. Spielman G, Gennarelli TA, Rogers CR. Disodium etidronate: its role in preventing heterotopic ossification in severe head injury. Arch Phys Med Rehabil. 1983;64(11):539-542.
Cite this Page
Links to the ERABI Clinical Tool may be used; however, that link cannot state or imply any sponsorship or endorsement of your website or content by the ERABI Clinical Tool, its members or any affiliated organizations. The ERABI logo should not be used at any time. When referencing specific content, ensure that the original source is referenced, if applicable. When ERABI Clinical Tool content is used it must be unaltered; please use the following citation: